I wrote this blog post with Naomi Murphy-King, Head of Delivery in PPS, to outline our strategic direction.
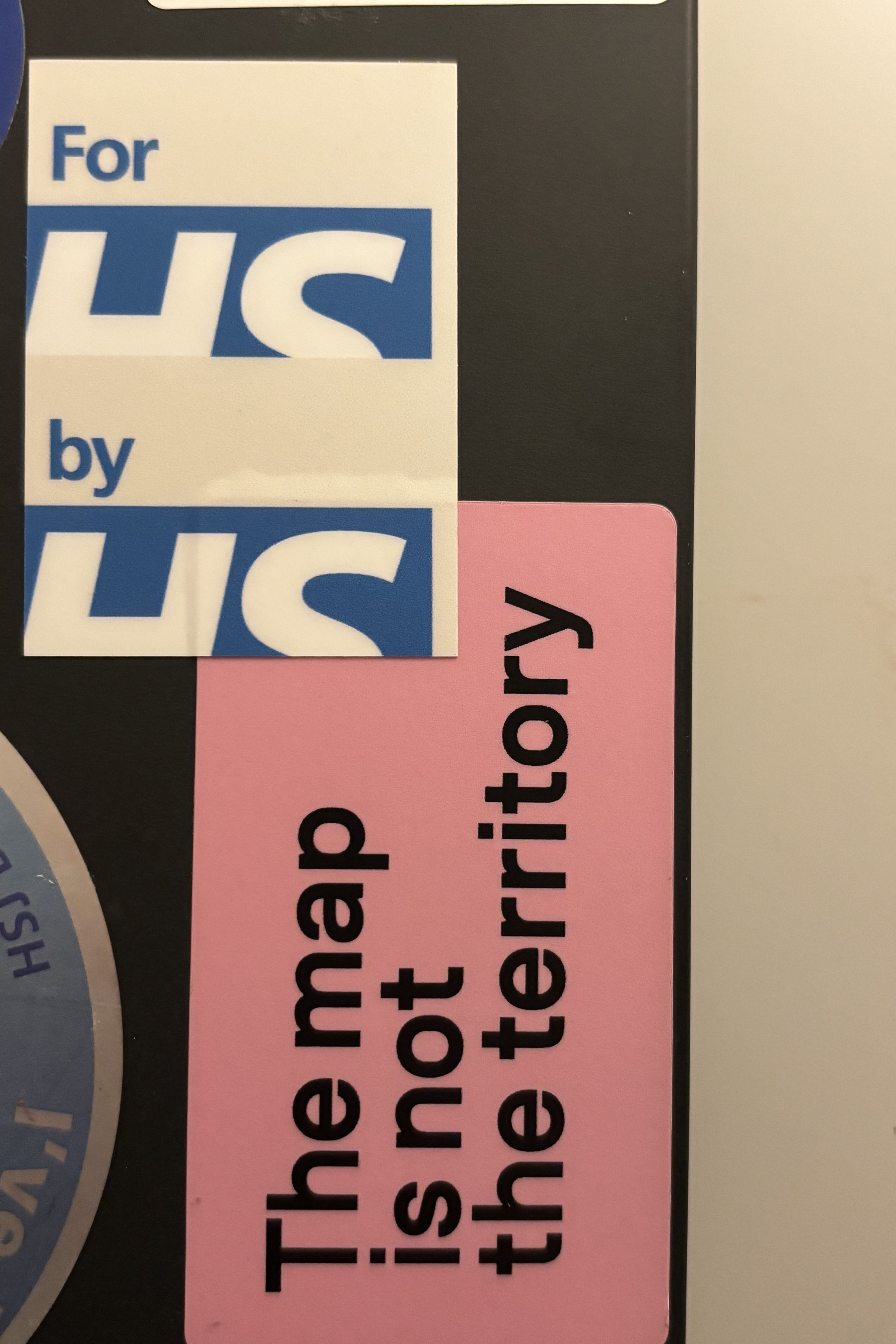
If this blog post is too long and you can’t be bothered to read it – these two stickers serendipitously placed next to each other on my laptop perfectly capture the essence of our strategy.
Recently we’ve been revisiting the Personalised Prevention Services (PPS) strategy to reflect our learnings from the past year, and to better signal our intent to our teams and to the wider environment – stakeholders and teams around us. We also hope to use a version of it to engage with the system and be tighter about our proposition.
Over the last few weeks we’ve been iterating it, talking to teams about it and getting feedback, playing it back to our DPSP leadership, and refining based on all the feedback we’re getting.
This has been less about writing a “perfect” strategy, and more about making our direction clearer and more representative of the needs we’ve uncovered.
What we’ve learned
In the past year since starting work on PPS, we’ve learned a lot about both the strategic context and what has worked (and not worked) in our delivery.
About the strategic context
Many prevention services, especially those that require behaviour change, are delivered at a local level.
Uptake of prevention services is low and declining. For example, uptake of NHS Health Checks is around 39%. People often do not know what is available, whether they are eligible, or how to access services. Current models often fail people who are excluded or experience the greatest health inequalities.
The 10 Year Plan sets clear ambitions to deliver on a personalised prevention vision, including the capabilities needed to support it. But delivering this ambition depends on enabling local areas to do the work.
Neighbourhood health is a priority. Our work therefore needs to support, and be mindful of, the changing ICB landscape and commissioning context. So we need to provide value in terms of health outcomes and efficiencies, in a complex system where local delivery is critical.
About our delivery landscape
We continue to deliver through a test and learn approach. We know that one of the riskiest assumptions we are trying to prove is whether people will act on the changes we recommend and support them to make. The only way to prove this is to do it for real.
However, we also need to be pragmatic. We have learned that some NHS England assurance requirements are constraints we must work within. To make progress, we need to build trust that we can prove value and deliver safe services, before we can influence those constraints to change. For example, we’ve recently recognised that our ‘Help to Stay Healthy’ product, which helps people connect to the right local prevention service for them, should go through a formal Alpha service assessment before we test it in the wild with a working code, real people and their all too real health outcomes.
Our strategy
As a reminder, our vision (which has now become DPSP’s vision) is:
To make it easy for people to understand their health risks and find the right services to stay well.
To realise this vision, PPS will help the system deliver prevention that feels joined up, intuitive and meaningful for people and healthcare providers.
We do this by building shared, reusable capabilities that help people stay healthier for longer.
We will provide infrastructure and end-user services that are available nationally and can be tailored to meet local needs. Our role is to be a system enabler, supporting ICBs, GP practices, providers and local authorities to transform how personalised prevention is delivered.
We help more people access more prevention services, where they are at.
For the NHS, by the NHS.
How do we do this?
By offering services, tools and capabilities that are too good not to adopt.
By working in multidisciplinary teams and partnering directly with policymakers, local services, ICBs and the wider healthcare system. This helps people find support that already exists in their communities and maintain healthier habits over time.
By starting small, with a limited number of local partners or use cases, to test and learn before exploring scale.
The services we want to test and offer
- Componentised health assessments that can be reused across services and areas to help people understand their health risks
- Seamless hybrid journeys for prevention and health assessment (digital and non-digital)
- Health risk calculation tools and infrastructure that integrates multiple risk factors
- Helping people connect to the prevention services and tools that best meet their needs and preferences
- Maintaining healthy habits through ongoing support and proven behavioural change support
In upcoming posts I’ll share more about each of these product areas and what we’re working on.
What next
We’ve been mapping how our longer-term vision translates into now, next and later time horizons. We are working with our teams to stress test proposals across the portfolio and ensure that what we are building now supports where we want to get to.
We are also doing Wardley mapping to better understand what we should and should not prioritise at a tactical level (more on that in a future weeknote). We will start sharing this work more widely with colleagues across DPSP, Products and Platforms, DHSC and beyond.
A lot feels clearer a year on from starting Personalised Prevention Services. And yet, as we start launching products live and engaging actively with users across the healthcare system, we’ll uncover a lot more data points that make us pivot, or at least gently course correct. So one thing will always be true for our strategy – the map is not the territory.
Do you have feedback or want to know more? Reach out to us via email or directly to us on LinkedIn.
Leave a comment